38/M with pain abdomen since 15 years
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio.
Case history:
History of present illness:
Patient had complaints of pain abdomen since 15years which is squeezing type, intermittent and diffuse. He also had episodes of loose stools and constipation over the past.
He also had complaints of retrosternal burning sensation and belching, episodes of blood in stools.
Then he visited local RMP with these complaints and was given medication for immediate relief. This continued for years.
Later, in 2015, patient had complaints of fever, cold, cough and was diagnosed with pulmonary TB. He was started on ATT and continued the medication for 6minths as advised by the doctor.
In 2019, he had similar complaints of fever, cough and was again diagnosed with TB. Used medication (ATT) for another 6months.
C/o pain abdomen did not subside over the years inspite of use of medication. He started losing weight and approached a doctor for these complaints and was diagnosed with ulcerative colitis and was prescribed medication. There was no improvement in the symptoms even after.
Past history-
Not a k/c/o DM ,HTN, TB,ASTHMA, CVA, CAD.
Personal history :
Diet :mixed
Appetite : decreased
Sleep : adequate
Bowel movements: constipation and blood in stools
Bladder movements:regular
Addictions: Alcoholic. Abstinent since 1 month.
Family history :
Not significant
General examination:
Patient is consious, coherent, cooperative.
No signs of icterus, pallor,clubbing, lymphadenopathy, edema.
Vitals:
Temp: 98.6 F
PR: 84 bpm
RR: 20 cpm
Grbs: 115 mg/dl
Spo2: 98%
Systemic examination
Per Abdomen
Inspection:
Skin - smooth
Shape - flat
Umbilicus - normal
Abdominal wall movements - present
No visible pulsations and peristaltic movements seen.
Palpation:
Tenderness - mild
No rise of temperature
No organomegaly
Percussion:
Tympanic note heard.
Auscultation :
Bowel sounds heard
No bruit.
CVS - S1, S2 heard, no murmurs.
CNS - NFND
RS - BAE present, NVBS heard
Sr. Creatinine -1.1
Hemogram:
Hb - 15
TLC - 7200
PLT - 3.77
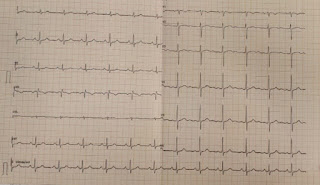
ECG:
CECT abdomen:
Diagnosis:
Malabsorption syndrome
Treatment:
IVF:NS@75ML/HR
PLENTY OF ORAL FLUIDS
INJ NEOMOL 1GM IVISOS
T.TAXIM 200MG PO/BD
TAB:RIFAGUT 550MG PO/BD
T PAN 40MG PO/OD
TAB SPOROLAC DS PO/BD
T.DOLO 850MG PO/BD
TAB BUSCOPAN PO SOS
CEBHYDRA LOTION FOR L/A BD
MOMATE CREAM L/A OD
OINT THROMBOPHOBE L/A




Comments
Post a Comment